The human heart is often described as a pump, but theres much more to it: it also has a special electrical system that regulates and coordinates heartbeats.Abnormal heartbeats are called arrhythmias, and probably the most common one isatrial fibrillation, a condition that affects millions of older adults and plays a major role in stroke, disability, and hospitalization.Some people with atrial fibrillation come to medical attention because they feel unwellshort of breath, fatigued, or aware that their heart is racing.Others feel fine and are surprised when a clinician or maybe even their smartwatch tells them they have an irregular heartbeat.Families are often left trying to understand a diagnosis that sounds ominous and a set of treatment options that can feel confusing or even frightening.To help clarify what matters most, I spoke with cardiologist and electrophysiologist Cara Pellegrini, MD, about atrial fibrillation in aging.
Heres what to know, including what atrial fibrillation is, why it matters, and how to think through treatment and stroke preventionespecially when frailty, falls, or cognitive impairment are part of the picture.Dr.Kernisan: What exactly is atrial fibrillation?Dr.Pellegrini:
Atrial fibrillation, or AFib, is a heart rhythm disorder.
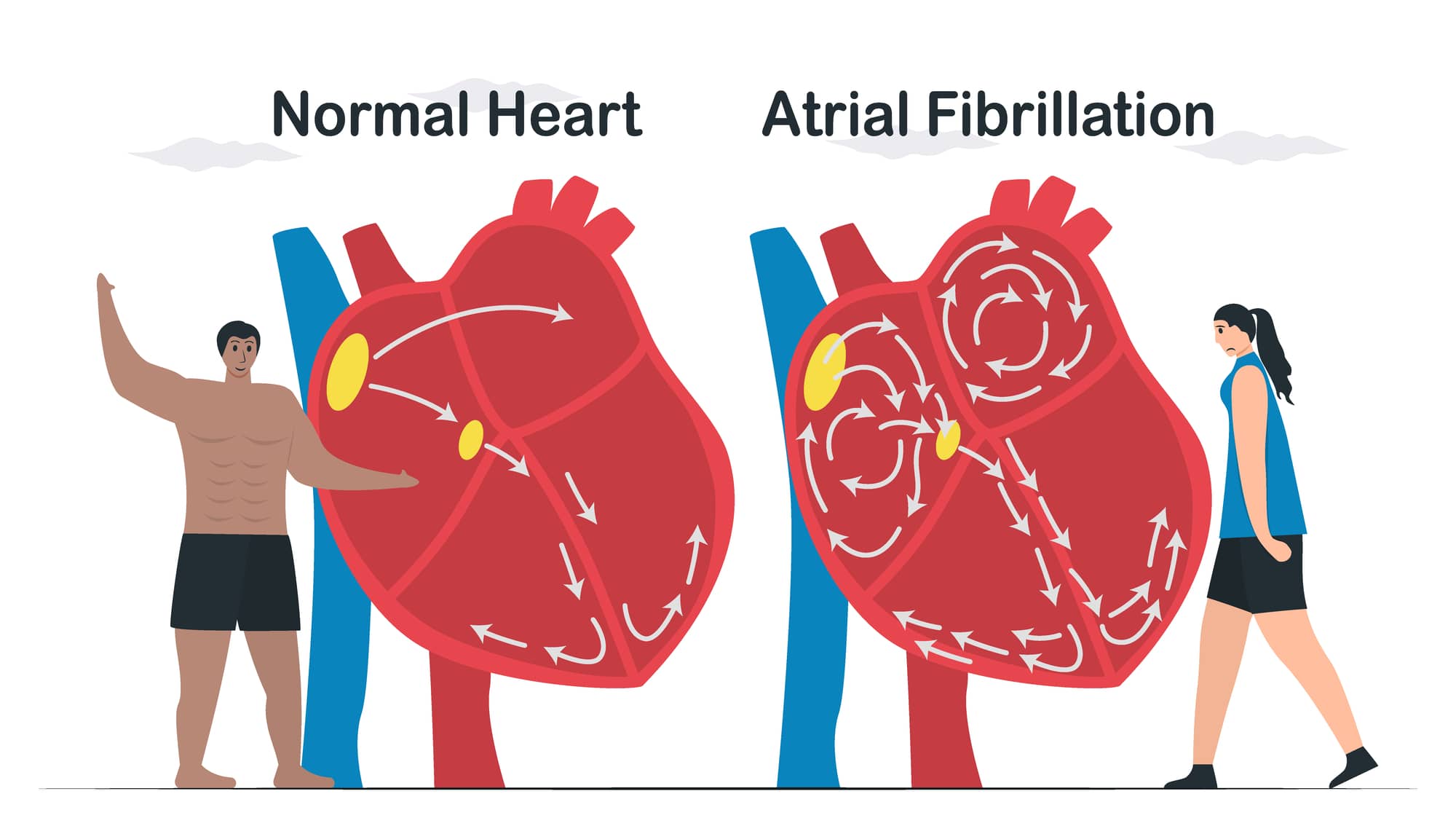
In a normal heart, each beat begins with an electrical signal from the sinus node in the upper chamber.That signal travels in an organized way through the heart, allowing the upper chambers to squeeze first and then the lower chambers to pump blood to the lungs and the rest of the body.In atrial fibrillation, the electrical activity in the upper chambers becomes chaotic.Instead of contracting normally, the atria quiver.
This leads to irregular electrical signals reaching the lower chambers, which then beat irregularly and often too fast.That irregular pulse is one of the hallmarks of atrial fibrillation.Dr.Kernisan: So atrial fibrillation is primarily an electrical problem?Dr.
Pellegrini:
Yes.Many people assume that any heart problem means blocked arteries or a weak heart muscle, but atrial fibrillation is fundamentally an electrical disorder.Someone can have atrial fibrillation with otherwise normal heart structure and pumping function.That said, electrical problems and structural problems often interact.
Atrial fibrillation can contribute to heart weakness over time, and heart disease can increase the likelihood of developing AFib.But its important to recognize that AFib itself is not the same thing as coronary artery disease.Dr.Kernisan: What causes atrial fibrillation, particularly in older adults?Dr.
Pellegrini:
Anything that stretches or scars the atria increases the likelihood of atrial fibrillation.Aging is one of the strongest risk factors, and unfortunately, its not modifiable.Other common risk factors for developing afib include:High blood pressureDiabetesObesityPhysical inactivitySleep apneaAlcohol useAlcohol is particularly important: regular drinking increases risk over time, and even a single episode of heavier drinking can trigger an AFib episode.The encouraging part is that many of these risk factors are modifiable.Addressing them can reduce the frequency of AFib episodes and sometimes slow or even partially reverse progression.Dr.
Kernisan: How common is atrial fibrillation in later life?Dr.Pellegrini:
It becomes increasingly common with age.By age 80 and older, roughly one in ten people has atrial fibrillation.
If someone lives long enough, the odds of developing it are quite high.This is why atrial fibrillation is such a major issue in geriatrics and primary careits not rare, and it affects a very large number of older adults.Dr.Kernisan: What symptoms do people experience?Dr.Pellegrini:
People in AFib have an irregular heart rate, but they may not notice it.
Symptoms vary widely.Many people, especially those who develop atrial fibrillation gradually, have no symptoms at all, but others do experience symptoms.Some common symptoms of AFib include:PalpitationsShortness of breathFatigueDizzinessReduced exercise toleranceFeeling mentally foggy or offDr.Kernisan: How is atrial fibrillation diagnosed?Dr.
Pellegrini:
The diagnosis requires an electrocardiogram, or ECG, which shows the electrical activity of the heart.An irregular pulse or a smartwatch alert raises suspicion, but an ECG is needed to confirm AFib and distinguish it from other rhythm issues.If atrial fibrillation comes and goes, we often use wearable monitors or patches that record heart rhythms over days or weeks.Its also important to evaluate for reversible causes, such as thyroid disease or acute illness, because treating those can sometimes resolve the problem.Dr.
Kernisan: Once AFib is diagnosed, how is it treated?Dr.Pellegrini:
In AFib treatment, we pursue several goals at the same time:How to help the person feel better (symptom control)How to protect the heart over timeHow to reduce stroke riskNot every patient needs treatment to restore a normal heart rhythm.Treatment should be individualized, especially in older adults.Dr.
Kernisan: Lets talk about symptom control first.Dr.Pellegrini:
If symptoms are mild or absent, we may focus on controlling the heart rate.This means allowing atrial fibrillation to continue but preventing the heart from beating too fast.
Keeping the heart rate in a reasonable range often improves fatigue, shortness of breath, and dizziness.For many older or frail adults, this approach works well and avoids more intensive interventions.Dr.Kernisan: What about rhythm control?Dr.Pellegrini:
Rhythm control aims to restore and maintain a normal heart rhythm.
This can involve medications, electrical cardioversion, or catheter ablation procedures.There is growing evidence that maintaining normal rhythm can benefit long-term heart health, but these strategies are more involved and not appropriate for everyone.Age, frailty, symptom burden, and personal goals all matter.Dr.Kernisan: How does frailty influence treatment decisions?Dr.
Pellegrini:
In frail older adults or those with limited life expectancy, we usually prioritize comfort and simplicity.If atrial fibrillation isnt causing symptoms, we may focus primarily on stroke prevention.If medications cause side effects and symptoms persist, one option is placing a pacemaker and ablating the AV node.This creates reliable rate control and can be very effective even in people with multiple medical problems.Dr.
Kernisan: Stroke prevention is often what worries families most.Why is AFib so strongly linked to stroke?Dr.Pellegrini:
When the atria arent squeezing effectively, blood can pool.
Most AFib-related clots form in a small outpouching called the left atrial appendage.A clot formed there can travel to the brain and cause a stroke.AFib-related strokes are often severe and disabling, which is why prevention is such a central focus of care.Dr.Kernisan: How do clinicians estimate stroke risk?Dr.
Pellegrini:
We use a risk score that takes into account age, high blood pressure, diabetes, heart failure, vascular disease, and prior stroke.For many older adults, untreated stroke risk is 2-8% per year.A commonly used risk calculator is the CHADS2-VASC.Reducing stroke risk by even a few percentage points matters because stroke can permanently change someones independence and quality of life.Dr.Kernisan: What role do blood thinners play?Dr.
Pellegrini:
Anticoagulants reduce stroke risk by about half.Today, we mostly use direct oral anticoagulants, such as apixaban (brand name Eliquis) or rivaroxaban (brand name Xarelto).They are easier to use and safer than older drugs like warfarin.Aspirin alone is no longer recommended for stroke prevention in atrial fibrillation.
It does not provide adequate protection.Dr.Kernisan: What are the downsides of anticoagulation, especially in older adults?Dr.Pellegrini:
The main downside is bleeding risk.
Anticoagulants make it harder for blood to clot everywhere in the body.This can lead to nuisance bleeding, such as easy bruising or prolonged bleeding from small cuts, as well as more serious bleeding in the gastrointestinal tract or brain.In geriatrics, falls are a major concern.If someone falls frequently and hits their head while on a blood thinner, the risk of serious bleeding is higher.
This creates a difficult balancing act, because stroke risk also increases with age.Dr.Kernisan: This brings us to the Watchman device.Can you explain what it is?Dr.
Pellegrini:
The Watchman device is designed to reduce stroke risk without lifelong systemic anticoagulation.It seals off the left atrial appendage, which is where most AFib-related clots form.The device is placed through a minimally invasive procedure using catheters inserted through the veins in the leg.Over time, the body grows tissue over the device, effectively closing off that pouch so blood cant pool there.Dr.
Kernisan: How does Watchman compare to blood thinners?Dr.Pellegrini:
After a healing period, Watchman provides stroke protection comparable to long-term anticoagulation.Initially, patients still need short-term blood thinners or antiplatelet therapy while the device heals in place.For people at high bleeding risk, this can be a very attractive option because it avoids lifelong exposure to anticoagulants.Dr.
Kernisan: Who should consider Watchman?Dr.Pellegrini:
We often consider it for people who have a high risk of bleeding, frequent falls, or a history of gastrointestinal bleeding.It can also be helpful for people who need medications like NSAIDs (e.g.
ibuprofen), which interact poorly with blood thinners.Most recipients are over age 75.Selected patients with mild dementia may be appropriate candidates if they have a reasonable life expectancy and goals of care that align with stroke prevention.Dr.Kernisan: How does dementia factor into these decisions?Dr.
Pellegrini:
Mild dementia does not automatically rule out Watchman.Many patients with mild cognitive impairment or early dementia can tolerate the procedure well.In advanced dementia, where life expectancy is limited and the focus is comfort, invasive procedures often no longer align with goals of care.As always, decisions should be individualized.Dr.
Kernisan: How important are lifestyle changes in managing atrial fibrillation?Dr.Pellegrini:
They are extremely important.Managing blood pressure, exercising regularly, reducing alcohol intake, maintaining a healthy weight, and treating sleep apnea can significantly reduce AFib burden.In some people, these changes can reduce AFib episodes or even partially reverse the condition.
This is very much a partnership between clinicians and patients.Dr.Kernisan: What questions should patients and families ask near the end of a visit?Dr.Pellegrini:
Some key questions include:What is my personal stroke risk, and how can we reduce it?What options are available to help me feel better day-to-day?How do my other medical conditions affect these treatment choices?What are the risks and benefits of blood thinners versus alternatives like Watchman?How often should we reassess these decisions as my health changes?Closing ThoughtsAtrial fibrillation is common in later life, but it is manageable.
With thoughtful, individualized care, many people live well for years.Understanding the condition and actively participating in decisions can make a meaningful difference.Note: This article is based on a video podcast interview and has been edited and condensed for clarity and readability.
Disclaimer: This story is auto-aggregated by a computer program and has not been created or edited by Senior Savings Deals.
Publisher: Better Health ( Read More )
Publisher: Better Health ( Read More )